What's all this fuss about our gut at the moment?
The suggestion that the bacteria naturally living (happily and relatively quietly) in out gut could contribute to our overall health and disease status began to emerge as a concept in around 2010. It has begun to gather serious momentum over the last few years on social media with 'Insta-celebs' posting about the benefits of eating fermented foods to 'rectify' or 'calm' gut bacteria. It is often discussed in relation to bowel conditions and food intolerances but for us there is a more interesting suggestion on how our gut bacteria may be heavily implicated in the development of autoimmune diseases.
The suggestion that the bacteria naturally living (happily and relatively quietly) in out gut could contribute to our overall health and disease status began to emerge as a concept in around 2010. It has begun to gather serious momentum over the last few years on social media with 'Insta-celebs' posting about the benefits of eating fermented foods to 'rectify' or 'calm' gut bacteria. It is often discussed in relation to bowel conditions and food intolerances but for us there is a more interesting suggestion on how our gut bacteria may be heavily implicated in the development of autoimmune diseases.
A quick word on terminology
This relatively recent upsurge in interest around the gut has inevitably piqued interest in the popular press and has muddied the water somewhat in terms of what exactly is being talked about. I have seen the terms 'microbiota' and 'microbiome' used seemingly interchangeably in some popular press so in the interest of clarity:
This relatively recent upsurge in interest around the gut has inevitably piqued interest in the popular press and has muddied the water somewhat in terms of what exactly is being talked about. I have seen the terms 'microbiota' and 'microbiome' used seemingly interchangeably in some popular press so in the interest of clarity:
- Microbiota: the collection of microbes within a specific anatomical niche (eg the lungs,genitals or gut). Over 70% of microbes (bacteria and viruses) within the body's total microbiota reside within the gut.
- Microbiome: all the genes derived from microbial processes occurring within the microbiota
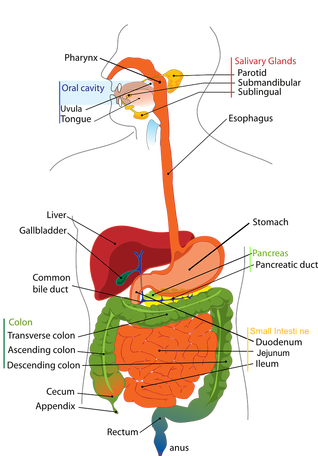
Where is our gut and what does it do?
Our gut - the long tube also called the digestive tract - runs from the mouth, down the gullet (oesophagus), through the stomach, small intestine, large intestine and anus, The gut is concerned with breaking down, processing, digesting and absorbing nutrients from food. Various organs are involved within this process from chewing and the action of digestive enzymes in the mouth; chemical breakdown and some absorption from the stomach; movement to the small and large intestine for further absorption and finally anything not absorbed by the body is expelled at the end of the tract (anus). This is not meant as a biology lesson but illustrates how large the gut area is and how important it is in its functioning.
Our gut - the long tube also called the digestive tract - runs from the mouth, down the gullet (oesophagus), through the stomach, small intestine, large intestine and anus, The gut is concerned with breaking down, processing, digesting and absorbing nutrients from food. Various organs are involved within this process from chewing and the action of digestive enzymes in the mouth; chemical breakdown and some absorption from the stomach; movement to the small and large intestine for further absorption and finally anything not absorbed by the body is expelled at the end of the tract (anus). This is not meant as a biology lesson but illustrates how large the gut area is and how important it is in its functioning.
The gut microbiota
The human gut plays host to trillions of bacteria and viruses which have tremendous potential to impact various facets of our health; they contribute metabolic functions, protect against pathogens and educate the immune system.
The composition of bacteria in our gut begins in utero and continues for the first 2-3 years of life. Recent studies have shown both short and longer-term effects on the composition of the microbiota in relation to:
The intricate composition of the gut has been described as our 'secondary genome' and is as individual as our genetic make-up. It lies in close association with with the host's (our) immune system and together plays a role in exerting various nutritional, metabolic and immunomodulatory functions important to our overall health and wellbeing.
The human gut plays host to trillions of bacteria and viruses which have tremendous potential to impact various facets of our health; they contribute metabolic functions, protect against pathogens and educate the immune system.
The composition of bacteria in our gut begins in utero and continues for the first 2-3 years of life. Recent studies have shown both short and longer-term effects on the composition of the microbiota in relation to:
- host genetics
- age
- external factors such as where and who we live with
- the use of pre- and pro-biotics
- exercise
- diet
The intricate composition of the gut has been described as our 'secondary genome' and is as individual as our genetic make-up. It lies in close association with with the host's (our) immune system and together plays a role in exerting various nutritional, metabolic and immunomodulatory functions important to our overall health and wellbeing.
Links between gut microbiota and disease
Research into the gut microbiota to date has shown this bacteria implicated in the development of diseases including:
Research into the gut microbiota to date has shown this bacteria implicated in the development of diseases including:
- type 1 diabetes
- irritable bowel syndrome (IBS)
- inflammatory bowel diseases (IBD)
- cardiovascular disease
- autoimmune diseases (including MS)
What do we currently understand about the possible implication of the gut in the mechanisms of these diseases?
The combination of different types of bacteria was shown to be imbalanced in individuals with these diseases. Some studies have shown this imbalance to be considerable in patients with MS with considerable under-representation of some bacteria and over-representation of others. The microbiota can be deeply influenced by external factors as mentioned earlier in this article, and its aim is to maintain equilibrium between the host (us) and the environment thus keeping an optimal balance of different bacteria.
Given the location and function of the gut diet has become the focus of much exploration. Dietary intake has been shown to be a key determinant in microbiome composition and diversity; this may have clinical implications here as evidence suggests composition of the microbiota in early life may be responsible for the programming of gastrointestinal , immune and neural development: key features in the diseases mentioned above.
How could this be relevant to my MS?
This may be pertinent here as when balance is maintained between the microbiome and metabolism of the host, all is well; when imbalance occurs inflammation and infection can result. As we know, in MS it is inflammation that is responsible for damage to the central nervous system; the symptoms we may present and the resulting build-up of disability.
I would love to tie this post up with a great dramatic conclusion (which might have been what you were waiting for - apologies), however this research in humans is at a relatively early stage so the conclusions aren't there yet. The hope is that in the future it can be used to develop further theraputic interventions and understand more about the fundamental mechanisms of disease development and progression.
A cautionary word (disclaimer)
This post began as an expected exploration of how diet can influence the gut (I'm aiming to alternate between diet and exercise each week in the blog posts). However this has turned into something much bigger that I have been interested in but haven't explored until now. I have no history within this area and I'm a little concerned that it is venturing out of what I set this blog up to share: ie things I know a lot about. So to be very transparent, this is a brief overview of some of the latest research papers; it is not a comprehensive literature review of all the research and conclusions produced to date. All the papers I have used to write this are referenced below so if you are hoping to use this for anything other than your own interest please consult one of the researchers working in the area; as always, consult an expert - this time, it's not me.
This post began as an expected exploration of how diet can influence the gut (I'm aiming to alternate between diet and exercise each week in the blog posts). However this has turned into something much bigger that I have been interested in but haven't explored until now. I have no history within this area and I'm a little concerned that it is venturing out of what I set this blog up to share: ie things I know a lot about. So to be very transparent, this is a brief overview of some of the latest research papers; it is not a comprehensive literature review of all the research and conclusions produced to date. All the papers I have used to write this are referenced below so if you are hoping to use this for anything other than your own interest please consult one of the researchers working in the area; as always, consult an expert - this time, it's not me.
References:
Adamczyk-Sowa,M. et al., (2017) ‘Does the gut microbiota influence immunity and inflammation in multiple sclerosis?’, Journal of Immunology Research, [epub ahead of print] doi: 10.1155/2017/7904821
Donovan, S.M. (2017) ‘Introduction to the special focus issue on the impact of diet on gut microbiota composition and function and future opportunities for nutritional modulation of the gut microbiome to improve human health’, Gut Microbes 8(2): 75-81
Glenn, J.D. and Mowry E.M., (2016) ‘Emerging concepts in the gut microbiome and multiple sclerosis’ Journal of Interferon and Cytokine Research 35(6): 347-357
Jangi, S. et al., (2016) ‘Alterations of the human gut microbiome in multiple sclerosis’, Nat Commun28(7): 1-11
Newland, P.K., Heitkemper, M. and Zhou, Y. (2016) ‘The emerging role of the gut microbiome in adult patients with multiple sclerosis’, J Neurosci Nurs 48(6): 358-364
Shailesh, S.K., Freedman, S.N and Mangalam, A.K. (2017) ‘Gut microbiome in multiple sclerosis: the players involved and the roles they play’, Gut Microbes July 11: 1-9 [epub ahead of print] doi: 10.1080/19490976.2017.1349041
Adamczyk-Sowa,M. et al., (2017) ‘Does the gut microbiota influence immunity and inflammation in multiple sclerosis?’, Journal of Immunology Research, [epub ahead of print] doi: 10.1155/2017/7904821
Donovan, S.M. (2017) ‘Introduction to the special focus issue on the impact of diet on gut microbiota composition and function and future opportunities for nutritional modulation of the gut microbiome to improve human health’, Gut Microbes 8(2): 75-81
Glenn, J.D. and Mowry E.M., (2016) ‘Emerging concepts in the gut microbiome and multiple sclerosis’ Journal of Interferon and Cytokine Research 35(6): 347-357
Jangi, S. et al., (2016) ‘Alterations of the human gut microbiome in multiple sclerosis’, Nat Commun28(7): 1-11
Newland, P.K., Heitkemper, M. and Zhou, Y. (2016) ‘The emerging role of the gut microbiome in adult patients with multiple sclerosis’, J Neurosci Nurs 48(6): 358-364
Shailesh, S.K., Freedman, S.N and Mangalam, A.K. (2017) ‘Gut microbiome in multiple sclerosis: the players involved and the roles they play’, Gut Microbes July 11: 1-9 [epub ahead of print] doi: 10.1080/19490976.2017.1349041